Audiovestibular medicine (formerly audiological medicine) is an expanding outpatient-based specialty, offering a range of clinical and intellectual challenges from physics to physiology and psychology.
Career satisfaction comes from making diagnoses and overseeing management of highly disabled and often neglected patient groups. The career structure is flexible and structured, offering good opportunities for combined posts, academic work or work-life balance.
Audiovestibular medicine trainee characteristics
Audiovestibular medicine will particularly suit trainees who are:
-
interested in complex medical problems
-
able to work with children and adults
-
good team players.
Training in audiovestibular medicine provides time for academic development, through strong support to complete a postgraduate diploma/masters degree in audiovestibular medicine.
-
Audiovestibular physicians are familiar with the execution and interpretation of a range of specialist investigations of the audiovestibular system.
-
Doctors can come to audiovestibular medicine with backgrounds in medicine, surgery or paediatrics. Tailored training is arranged to ensure the full range of competencies for the different backgrounds of trainees.
-
Consultant audiovestibular physicians work in a variety of settings, from community based clinics through secondary care and highly specialist academic centres.
Working in audiovestibular medicine
Audiovestibular medicine (AVM) is an exciting and tremendously varied specialty.
The core role of an audiovestibular physician is in the diagnosis, investigation and management of hearing and balance disorders. Typical patients will have problems such as hearing loss, tinnitus, dizziness, imbalance, eye movement disorders and speech problems.
Recent advances in technology (cochlear implants) and national initiatives (Newborn Hearing Screening) have broadened the specialty.
Audiovestibular physicians need excellent clinical and interpersonal skills, as many conditions are complex and long-term.
Audiovestibular physicians have a good understanding of the basic science underpinning hearing and balance, which they can apply to mechanisms of disease, and interpret for an individual. As the conditions seen are frequently chronic disorders, psychological and social aspects are frequently encountered and dealt with.
It is currently an excellent time to consider AVM as a career. The RCP has recognised the patchy provision of hearing and balance services around the country, and the need to gain more specialists to develop these services in areas that are currently under-resourced.
Further information
General / application queries
For general queries relating to areas such as eligibility criteria, making an application or the Oriel system, please contact the Physician Specialty Recruitment Office.
Queries regarding the progress of a submitted application should be directed to the lead recruiter for this specialty:
| London Recruitment Office | ||||||
|---|---|---|---|---|---|---|
| HST/general queries | General enquiries - Enquiry Form | |||||
| Fitness to practise- confidential | Fitness to practise form | |||||
Sometimes participates in round 2
This specialty’s participation in the second round is uncertain until after the first round is completed. Participation in the second round is confirmed in June each year.
Group 2 specialty
This is a Group 2 specialty and requires completion of the first two years of the internal medicine training (IMT) stage 1 programme or equivalent. Please visit the am I eligible? section of this website for further information about the eligibility criteria for Group 2 specialties.
Please be aware that audiovestibular medicine accepts applicants from other training routes, in addition to core-level physician training: general practice, otolaryngology (ENT) and paediatrics.
Non-physician applicants must have obtained the basic specialty professional examination in addition to specific clinical experience and competences to be eligible.
Please view the specialty's person specification for information about the requirements for applying from a non-physician background and the deadlines for when this must be achieved.
Current UK paediatric resident doctors
Person specifications state that completion of the required level of training for those currently in training, must be completed by the advertised post start date; which is early August for Round 1 and early February for Round 2. As all UK paediatric training programmes rotate in September and March, an exception will be made for those currently in ST3 training and due to complete that level within a month of the advertised post start date.
Applicants in this position can answer the application form on the basis of completing training by the advertised post start date, even though this will be up to a month after what is published. No further extensions will be permissible and this is purely to account for the UK-wide standard rotation dates of this specialty.
Commitment to specialty
The specialty will not be assessing your commitment to specialty as part of the shortlisting process and will score your application purely via the self-assessment scoring framework. Commitment to specialty will be assessed as part of the interview.
As part of the process of applying to HST, you may wish to gain an idea of how recruitment progressed in previous years for the various specialties participating in the nationally-coordinated recruitment.
To this end, we have published data dating back to 2013 (where this is available), based around four main areas:
-
Competition ratios - application numbers submitted to each specialty, along with the number of NTN and LAT posts available in each. It is worth noting that posts are subject to change throughout the round (increasing on average between 20-40%), and post numbers for this data are taken at the end of the round.
-
Shortlist scores - the scores awarded to all submitted applications, including average scores and distribution nationally.
-
Total scores - the total score awarded to all candidates who completed the full recruitment process for a specialty (application and interview), including some analysis of scores.
-
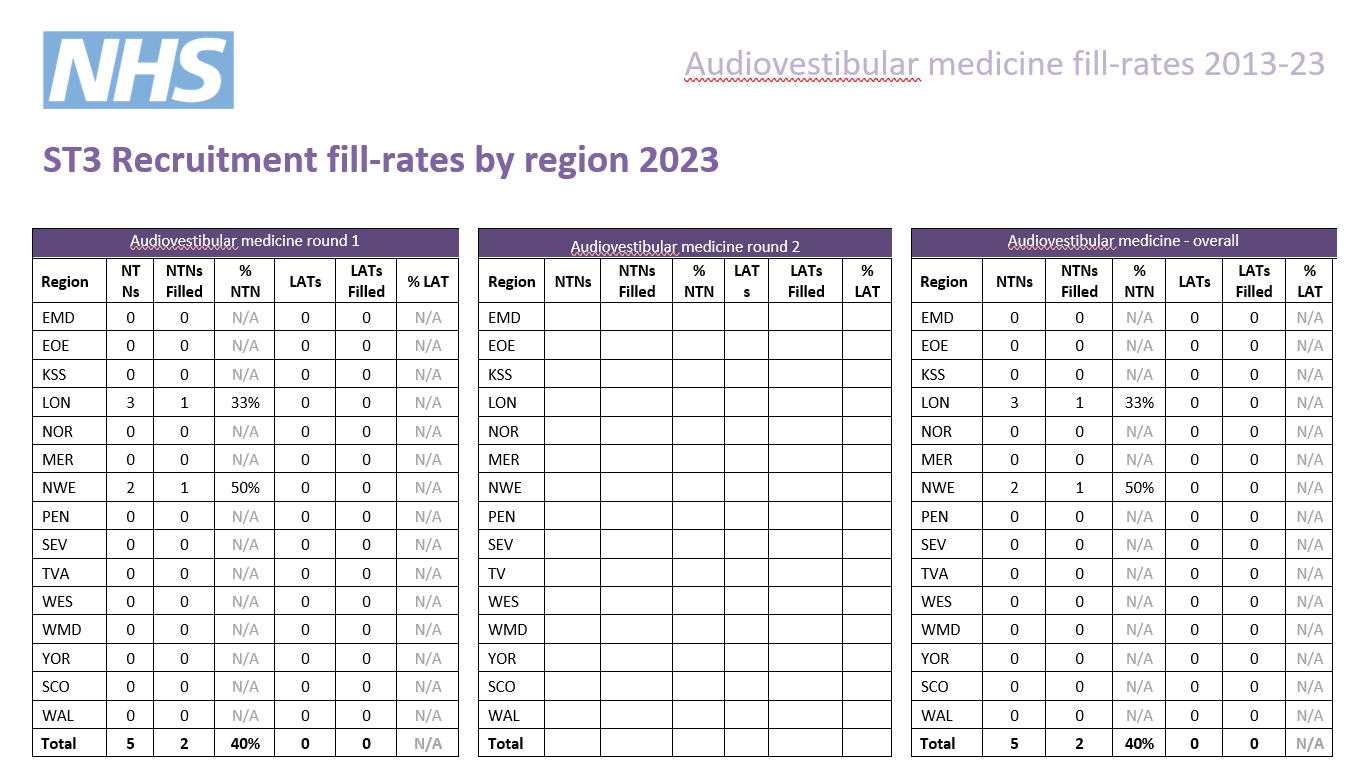
Post fill rates - the number of posts filled by region.
We have published information for all specialties participating in our process that year; consequently not all specialties will have data in all cases.
Round 1
| Year | Apps. | NTN posts | LAT posts | Total posts | Comp. | Unique* |
|---|---|---|---|---|---|---|
| 2025 | 32 | 2 | 0 | 2 | 16 | 44% |
| 2024 | 22 | 4 | 0 | 4 | 5.5 | 55% |
| 2023 | 6 | 5 | 0 | 5 | 1.2 | 67% |
| 2022 | 9 | 4 | 0 | 4 | 2.25 | 89% |
| 2021 | 12 | 4 | 0 | 4 | 3 | N/A** |
| 2020 | 9 | 6 | 0 | 6 | 1.5 | 56% |
| 2019 | 7 | 6 | 0 | 6 | 1.2 | 57% |
| 2018 | 9 | 3 | 0 | 3 | 3 | 78% |
| 2017 | 9 | 1 | 0 | 1 | 9 | 67% |
| 2016 | 10 | 2 | 0 | 2 | 5 | 90% |
| 2015 | 10 | 2 | 0 | 2 | 5 | 80% |
* the percentage of unique candidates that only applied to this specialty (out of the PSRO-coordinated specialties)
** As many specialties did not participate in recruitment in 2021, the data is not comparable.
Round 2
| Year | Apps. | NTN posts | LAT posts | Total posts | Comp. |
|---|---|---|---|---|---|
| 2023 | 9 | 5 | 0 | 5 | 1.8 |
| 2022 | 5 | 3 | 0 | 3 | 1.6 |
| 2021 | 5 | 4 | 0 | 4 | 1.25 |
| 2020 | 8 | 5 | 0 | 5 | 1.6 |
| 2019 | 1 | 5 | 0 | 5 | 0.2 |
Indicative post numbers
Indicative vacancy numbers are available in the table below, broken down by region and divided between substantive national training number (NTN) and locum appointment for training (LAT) posts. In many cases these will be presented as a range (e.g. 1-4) as it is not always possible for regions to know at this stage how many vacancies there will be.
It is the intention that indicative post numbers for all regions will be published prior to the application opening date, although this cannot be guaranteed. Please note that this table is not likely to be updated subsequent to indicative numbers and actual numbers will be confirmed when programme preferences are opened later in the round.
Numbers subject to change
Please be aware that it is not uncommon for vacancy numbers to change as the round progresses.
More commonly, post vacancy numbers can increase as the round goes on (and confirmation of posts becomes available); but it is also possible that numbers can reduce as well. In the past, post numbers have risen an average of 20-40% from the start to the finish of the round but this can vary greatly for individual specialty/region combinations.
It is possible that regions which do not have a post at the start of the round may declare one after applications have closed. Whilst we try and minimise instances of this, it is not always possible to predict vacancies so even if there appears not to be a vacancy in your preferred specialty/region combination, you may wish to consider applying in case one becomes available during the round; you can check with the region concerned if you wish to check on the likelihood of a post arising.
Generally, once a region enter a post into a round they would always have at least one post available and would only withdraw it in exceptional circumstances.
Round 1 Interview dates & post numbers
| Region | NTN posts | LAT posts* | Evidence upload date(s) | Interview date(s) |
|---|---|---|---|---|
| East Midlands | TBC | N/A |
29/12/25 - 12/01/26 |
26 February 2026 |
| East of England | TBC | N/A | ||
|
London |
0 - 1 |
N/A | ||
|
KSS |
N/A |
N/A |
||
| North East | TBC | N/A | ||
| North West (North West & Mersey) | 0 | N/A | ||
|
South West |
Peninsula |
N/A | ||
|
Severn |
N/A | |||
| Thames Valley | TBC | N/A | ||
| Wessex | TBC | N/A | ||
| West Midlands | TBC | N/A | ||
| Yorkshire & Humber | TBC | N/A | ||
| Wales | TBC | TBC |
*English LATs
Please note, English regions do not recruit to LAT posts.
**Scotland post numbers
If you are interested in working in Scotland, a breakdown of post numbers by the four Scottish regions is available on the Scottish Medical Training website. This has details of all specialty training post numbers in Scotland, including specialties which are not part of the nationally-coordinated process.
The SMT website will always be the more accurate one where they differ.
Interview Content
The interview will be split across two stations with a separate pair of interviewers scoring you on the areas in their station. The interview will consist of four questions which are each 10 minutes in length. You will be marked on these four questions and your communication skills, giving five scored areas in total. You will be scored by two interviewers in each station.
Each station will last 20 minutes, so, including the time between stations, the interview will be approximately 50 minutes.
Please note that this is subject to change and will be confirmed by the date of interview.
Prior to this question you will be given a clinical scenario and a short while to review it. You will then be asked questions relating to this scenario. Your communication skills will only be assessed during this question and marked accordingly. This question will last approximately 10 minutes.
The clinical scenario will be relatively brief (two/three sentences), so once you have seen this, the remainder of the preparation time will allow you to undertake some short mental preparation. Whilst it is permitted to make notes, these must be destroyed as soon as your interview is completed and not shared with anyone.
Clinical scenario considerations
The scenario will describe a hypothetical clinical situation which has arisen in which you are, or have become, involved. Some points to consider when reviewing the scenario and preparing for discussion are:
- what steps you would take
- any potential treatments possible
- any further information you would gather
- how you would go about communicating with any people (eg patients, family members, colleagues) involved in the scenario
You should also consider any other factors you deem appropriate, using your experience and professional judgement.
Areas for assessment
One mark will be awarded to you based on your suggestions and responses to the clinical scenario. The second mark will be on the communication skills you display.
This will be both an assessment of how you would communicate with patients, colleagues, etc. in the scenario, as well as of how well you communicate with interviewers.
This question will explore ethical, professionalism and governance issues. It will start with a hypothetical situation which is not given to you before entering the station and will be given verbally by interviewers.
This is not a clinical question, but will deal with the moral, ethical, legal, etc. issues of a particular situation. Following the hypothetical situation, and where time allows, there will be one or more questions about GMC Good Medical Practice principles.
The assessment of this question is underpinned by the principles of GMC Good Medical Practice.
This question will last approximately 10 minutes.
This question will see you given an ethical scenario to review. As with the clinical scenario at question 1, this takes the form of a hypothetical situation, described briefly in text form, details of which will be given to you prior to the question and you will have a short while to review it.
This scenario focuses less on a clinical situation, and deals more with consideration of the moral, ethical, legal (etc.) issues which may arise in a particular situation.
The area of assessment here will be your suggested responses to the ethical scenario during discussion, as well as your knowledge of the different considerations required.
This question will focus on your suitability for and commitment to training in the specialty and give you opportunity to expand on the information provided in your application form.
This question will last approximately 10 minutes.
Scoring framework
The score of 1-5 an interviewer will award you for each assessment area is judged in relation to how well you perform against an expected level. Below is the framework used to award scores at interview, as well as interpretation of what these scores represent:
|
Mark
|
Rating
|
Assessment
|
|
1 |
poor |
not considered appointable |
|
2 |
area for concern |
performed below the level expected from a core level trainee applying to the specialty; |
|
3 |
satisfactory |
performed at the level expected of a core level trainee applying to the specialty; |
|
4 |
good |
above average ability; |
|
5 |
excellent |
highly performing trainee; |
As shown in the table, for each of the question areas at interview, 3/5 is considered a satisfactory score; and reflects the level of performance that would be expected of a trainee ready to progress to a specialty training programme.
Should your performance go above and beyond this expected level, interviewers can award marks of 4/5 or 5/5 as appropriate.
Conversely, should your interview performance not reach the expected level, then interviewers can award marks of 1/5 or 2/5, as reflects their level of concern over your performance.
Appointability
Raw interview score (RIS)
The RIS is the sum of all ten scores awarded to you during your interview, but before any weighting is applied.
As each individual score will be between 1 and 5, your RIS will be between 10 and 50.
Appointability requirements
To be classed as 'appointable', you must meet all three criteria below:
- none of your ten interview scores can be 1/5
- no more than two of your ten interview scores can be 2/5
- your RIS must be 30 or above.
If you meet all three requirements, your application will be assessed as appointable, and can progress to be considered for post offers.
However, if you fail to meet any of these requirements, your application must then be assessed as not appointable, and it will progress no further in that round.
Total score
After interview, a weighting is applied to the scores in each area, as well as your application score.
These scores are then combined to give your total score which determines your ranking, which will in turn be used to inform how offers are made. The weighting of different sections, as well as the method by which your total score is established, is detailed in the table accessible through the link below:
|
|
Interviewer 1
|
Interviewer 2
|
Weighting
|
Max score
|
|
Question 1 |
||||
|
Clinical scenario |
/ 5 |
/ 5 |
2.0 |
20 |
|
Communication |
/ 5 |
/ 5 |
1.5 |
15 |
|
Question 2 |
||||
|
Professionalism and Governance |
/ 5 |
/ 5 |
1.5 |
15 |
|
Question 3 |
|
|
|
|
|
Ethical scenario |
/ 5 |
/ 5 |
1.0 |
10 |
|
Question 4 |
||||
|
Suitability and commitment |
/ 5 | / 5 | 2.0 | 20 |
|
Raw interview score |
/ 50 |
|||
|
Interview score (w weighting) |
/ 80 |
|||
|
Application score |
/ 40 |
0.5 |
/ 20 |
|
|
Total score |
/ 100 |
|||