Clinical Pharmacology and Therapeutics (CPT) is a dynamic specialty at the heart of patient care that makes a major contribution to the health and wealth of the nation. The core role of a clinical pharmacologist is to improve the care of patients (and indeed whole populations) through the safe, effective and efficient use of medicines. Training is combined with general internal medicine (GIM) leading to a dual accreditation in CPT & GIM.
CPT trainee characteristics:
CPT will particularly suit trainees who:
- Show good team-player and leadership skills, especially those aspiring to future clinical leadership roles
- enjoy variety in training (including beyond the ward and outpatient clinic)
- are keen to disseminate knowledge through teaching, training and presentations
- have the ability to work (and enjoy working) under pressure.
- are keen to engage in experimental, translational and/or clinical research (although prior experience of research is not essential)
Working in CPT:
Embark on a consultant career where in addition to delivering clinical care your specialist expertise influences policy, shapes guidelines, and contributes to the strategic direction of healthcare. CPT offers a fulfilling journey for those seeking a career that goes beyond the ward, clinic and prescription pad, making a lasting impact on patient care and healthcare systems.
As a small specialty, unless you have met some of us, you might never have heard of CPT or be unclear about the scope of our practice. The wide variability in CPT consultant job plans further adds to the mystery, making it less visible compared to more mainstream specialties. Follow the links below in the section called ‘Links’ to the British Pharmacology Website for lots more information on careers in CPT.
Clinical Pharmacologists improve patients’ lives by developing new medicines, by ensuring they are used safely and effectively, and by providing general and specialist medical services, often as part of a multidisciplinary team of healthcare professionals, working in hospitals, academia, the pharmaceutical industry and the community.
Clinical Pharmacologists ensure there is an overarching, cross-specialty stewardship of all aspects of medicines used in the NHS and do so by:
1. Specialist and generalist patient care including managing patients with complex prescribing needs including; polypharmacy, adherence and intolerance; preventing and managing adverse drug reactions; identifying and reducing medication errors; managing patients with poisoning, hypertension or other conditions requiring specialist therapeutics knowledge and skills; facilitating the transition to precision medicine, including individualised pharmacogenomic-based prescribing; and providing acute and general medical care.
2. Medicines policy and management including; providing leadership in ensuring the safe and optimal use of medicines within the health service at local, regional and national levels including the promotion of collaboration with other specialties and pharmacy; leading for medicines regulation and health economic assessments; producing prescribing guidance and medicines optimisation policy.
3. Education and training Teaching is at the core of our specialty, with Clinical Pharmacologists actively involved in educating the next generation of healthcare professionals. From medical students to fellow practitioners, our community fosters a culture of continuous learning and knowledge dissemination, particularly in relation to all aspects of the safe, effective and economic use of medicines.
4. Development of medicines and other therapeutics, including; designing and leading safe and effective clinical trials, including first-in-human studies; working with the life sciences industry to discover new medicines, explore their efficacy, repurposing potential and adverse effects; bridging the translational gap between basic science and clinical practice; leading for pharmacovigilance of licensed medications; and leading NHS research facilities. Our specialty bridges the gap between bench science and clinical application, fostering a holistic approach to patient care.
Why not explore the new CPT curriculum that reflects the evolving landscape of medicine, ensuring our practitioners are equipped with cutting-edge knowledge and skills, by following the link below?
Delve into the diverse facets of Clinical Pharmacology and Therapeutics, where specialists thrive in roles ranging from Clinical Toxicologist for the National Poisons Information Service to Early Phase Clinical Trial design and delivery, from working as experts for the MHRA or NICE to teaching core pharmacology and prescribing to students and healthcare colleagues. Our experts lead in tackling clinical challenges like hypertension, ensuring optimal medicines management and governance locally, nationally and regionally, and navigating complexities related to polypharmacy and adverse drug effects.
Further information
- For personal accounts of careers in CPT (including 'day-in-the-life'-style accounts), please visit the British Pharmacological Society website
- Beyond Medical School | British Pharmacological Society (bps.ac.uk)
- NHS health careers
- JRCPTB specialty page and curriculum
- ST4 CPT person specification
General / application queries
For general queries relating to areas such as eligibility criteria, making an application or the Oriel system, please contact the Physician Specialty Recruitment Office.
Queries regarding the progress of a submitted application should be directed to the lead recruiter for this specialty. The lead recruiter for clinical pharmacology and therapeutics is East of England.
| NHS England East of England | ||||||
|---|---|---|---|---|---|---|
| email address | ||||||
Expected to participate in round 2
This specialty has traditionally participated in the second round. Although it cannot be guaranteed until the first round is completed, it is very likely that there will be a second round for this specialty this recruitment year. Participation in the second round is confirmed in June each year.
Group 1 specialty
This is a Group 1 specialty and requires completion of the internal medicine training (IMT) stage 1 programme or equivalent; all programmes in the specialty will dual specialise with general internal medicine.
Therefore, this specialty uses the standard HST eligibility criteria for Group 1 specialties and does not accept candidates from any alternative training routes. Please visit the am I eligible? section of this website for further information.
Commitment to specialty
The specialty will not be assessing your commitment to specialty as part of the shortlisting process and will score your application purely via the self-assessment scoring framework. Commitment to specialty will be assessed as part of the interview.
As part of the process of applying to HST, you may wish to gain an idea of how recruitment progressed in previous years for the various specialties participating in the nationally-coordinated recruitment.
To this end, we have published data dating back to 2013 (where this is available), based around four main areas:
-
Competition ratios - application numbers submitted to each specialty, along with the number of NTN and LAT posts available in each. It is worth noting that posts are subject to change throughout the round (increasing on average between 20-40%), and post numbers for this data are taken at the end of the round.
-
Shortlist scores - the scores awarded to all submitted applications, including average scores and distribution nationally.
-
Total scores - the total score awarded to all candidates who completed the full recruitment process for a specialty (application and interview), including some analysis of scores.
-
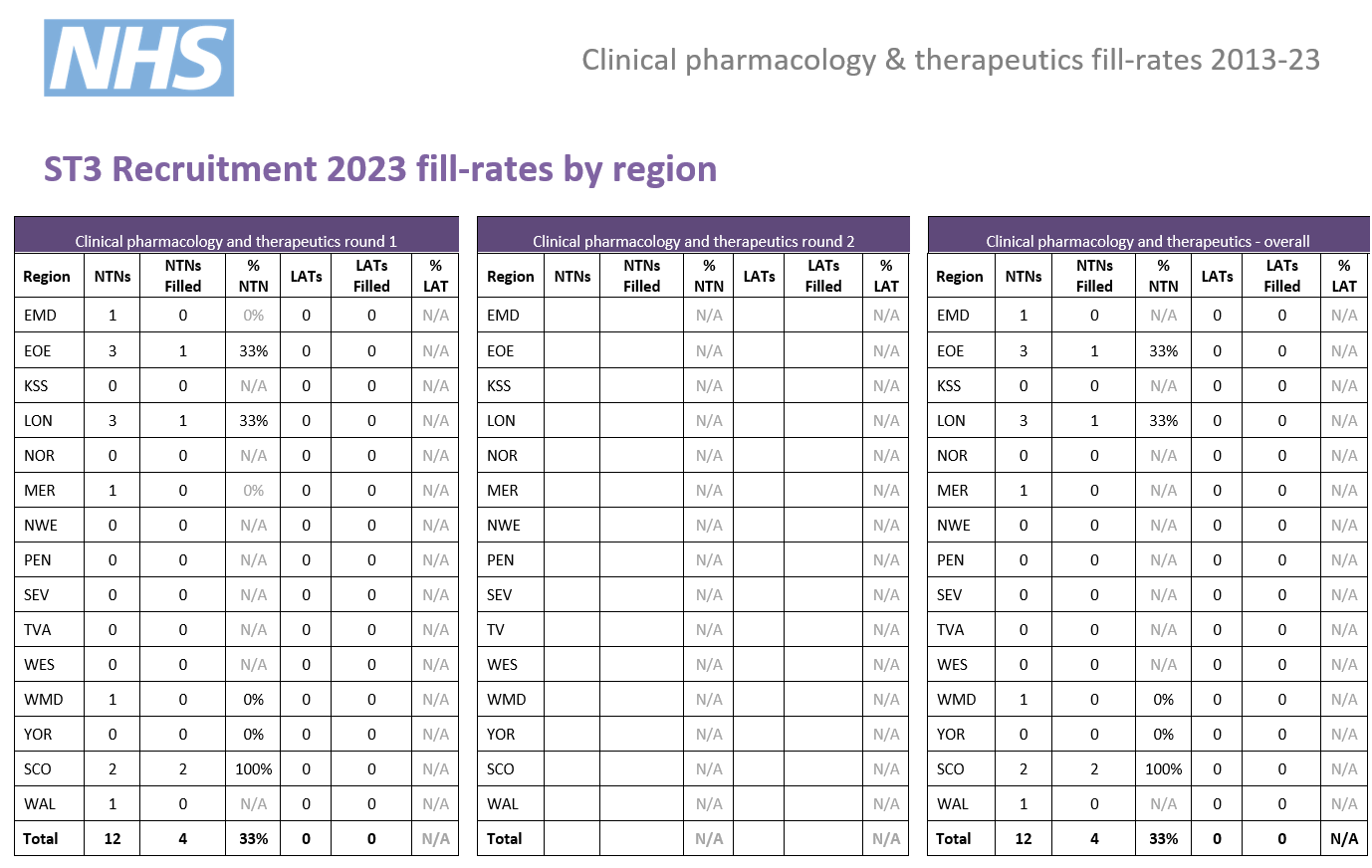
Post fill rates - the number of posts filled by region.
We have published information for all specialties participating in our process that year; consequently not all specialties will have data in all cases.
Round 1
| Year | Apps. | NTN posts | LAT posts | Total posts | Comp. | Unique* |
|---|---|---|---|---|---|---|
| 2025 | 16 | 8 | 2 | 10 | 1.6 | 0% |
| 2024 | 23 | 5 | 0 | 5 | 4.6 | 13% |
| 2023 | 25 | 12 | 0 | 12 | 2.1 | 28% |
| 2022 | 24 | 9 | 0 | 9 | 2.7 | 0% |
| 2021 | Did not participate in round 1 | |||||
| 2020 | 12 | 13 | 1 | 14 | 0.9 | 17% |
| 2019 | 14 | 12 | 0 | 12 | 1.2 | 21% |
| 2018 | 14 | 13 | 1 | 14 | 1.0 | 50% |
| 2017 | 9 | 15 | 0 | 15 | 0.6 | 22% |
| 2016 | 10 | 7 | 2 | 9 | 1.1 | 10% |
| 2015 | 8 | 9 | 0 | 9 | 0.9 | 50% |
* the percentage of unique candidates that only applied to this specialty (out of the PSRO-coordinated specialties)
Round 2
| Year | Apps. | NTN posts | LAT posts | Total posts | Comp. |
|---|---|---|---|---|---|
| 2024 | Did not participate in round 2 | ||||
| 2023 | 7 | 4 | 0 | 4 | 1.75 |
| 2022 | 4 | 8 | 3 | 11 | 0.3 |
| 2021 | Did not participate in round 2 | ||||
| 2020 | 17 | 6 | 0 | 6 | 2.8 |
| 2019 | 4 | 6 | 0 | 6 | 0.6 |
| 2018 | 5 | 11 | 0 | 11 | 0.5 |
| 2017 | Did not participate in round 2 | ||||
| 2016 | 3 | 6 | 0 | 6 | 0.5 |
| 2015 | 5 | 8 | 0 | 8 | 0.6 |
Indicative post numbers
Indicative vacancy numbers are available in the table below, broken down by region and divided between substantive national training number (NTN) and locum appointment for training (LAT) posts. In many cases these will be presented as a range (e.g. 1-4) as it is not always possible for regions to know at this stage how many vacancies there will be.
It is the intention that indicative post numbers for all regions will be published prior to the application opening date, although this cannot be guaranteed. Please note that this table is not likely to be updated subsequent to indicative numbers and actual numbers will be confirmed when programme preferences are opened later in the round.
Numbers subject to change
Please be aware that it is not uncommon for vacancy numbers to change as the round progresses.
More commonly, post vacancy numbers can increase as the round goes on (and confirmation of posts becomes available); but it is also possible that numbers can reduce as well. In the past, post numbers have risen an average of 20-40% from the start to the finish of the round but this can vary greatly for individual specialty/region combinations.
It is possible that regions which do not have a post at the start of the round may declare one after applications have closed. Whilst we try and minimise instances of this, it is not always possible to predict vacancies so even if there appears not to be a vacancy in your preferred specialty/region combination, you may wish to consider applying in case one becomes available during the round; you can check with the region concerned if you wish to check on the likelihood of a post arising.
Generally, once a region enter a post into a round they would always have at least one post available and would only withdraw it in exceptional circumstances.
Round 1 Interview dates & posts
|
Region
|
NTN posts
|
LAT posts*
|
Evidence upload date(s) | Interview date(s) |
|---|---|---|---|---|
|
East Midlands
|
0 - 1 | N/A |
13/01/26 - 30/01/26
|
12 March 2026 |
|
East of England
|
0 | N/A | ||
|
London
|
2 - 5 |
N/A | ||
|
Kent, Surrey and Sussex
|
TBC |
N/A | ||
|
North East
|
0 - 1 | N/A | ||
|
North West
|
0 - 1 |
N/A | ||
|
South West
|
Peninsula
TBC
|
N/A | ||
|
Severn
TBC
|
N/A | |||
|
Thames Valley
|
TBC | N/A | ||
|
Wessex
|
N/A | N/A | ||
|
West Midlands
|
0 - 1 | N/A | ||
|
Yorkshire & Humber
|
TBC | N/A | ||
|
Scotland**
|
2 |
TBC
|
||
|
Wales
|
TBC |
TBC
|
*English LATs
Please note, English regions do not recruit to LAT posts.
**Scotland post numbers
If you are interested in working in Scotland, a breakdown of post numbers by the four Scottish regions is available on the Scottish Medical Training website. This has details of all specialty training post numbers in Scotland, including specialties which are not part of the nationally-coordinated process.
The SMT website will always be the more accurate one where they differ.
Interview content
The interview will be split across two stations with a separate pair of interviewers scoring you on the areas in their station. There will be four questions which are 10 minutes each in length. You will be marked on these questions and your communication skills in both stations, giving six scored areas in total. The headings below show the question areas and in which station they will be covered, along with information about what will be assessed.
Each station will last 20 minutes, so, including the time between stations, the interview will be approximately 50 minutes.
Please note that this is subject to change and will be confirmed by the date of interview.
Prior to this question you will be given a clinical scenario and a short while to review it. You will then be asked questions relating to this scenario. This question will last approximately 10 minutes.
The clinical scenario will be relatively brief (two/three sentences), so once you have seen this, the remainder of the preparation time will allow you to undertake some short mental preparation. Whilst it is permitted to make notes, these must be destroyed as soon as your interview is completed and not shared with anyone.
Clinical scenario considerations
The scenario will describe a hypothetical clinical situation which has arisen in which you are, or have become, involved. Some points to consider when reviewing the scenario and preparing for discussion are:
- what steps you would take
- any potential treatments possible
- any further information you would gather
- how you would go about communicating with any people (eg patients, family members, colleagues) involved in the scenario
You should also consider any other factors you deem appropriate, using your experience and professional judgement.
This question will explore the non-clinical aspects of being a medical registrar, focusing on two of the Capabilities in Practice (CiPs) from the Internal Medicine Stage 1 Curriculum:
- Managing an acute unselected take
- Managing a multi-disciplinary team including effective discharge planning
You are required to start the station with a one-minute presentation: ‘A summary of your experience managing the acute unselected medical take as the medical registrar.’ In describing your experience, your presentation should summarise the following:
- The roles and duration you have undertaken in this capacity
- The level of responsibility you have held, and the degree to which you have been supervised
- The size and profile of the multi-disciplinary teams you have managed
- The number of patients for which you were directly and indirectly responsible whilst leading the acute unselected medical take
- Outline of the non-clinical duties you have performed in the role.
Following your presentation, interviewers may ask questions to clarify or ask you to expand upon your experience.
The remaining time in the station will ask you to draw on your experience of managing a team caring for acute medical admissions by giving examples of how you have managed different situations.
This question will last approximately 10 minutes.
Presentation guidance
When preparing your presentation, please bear in mind the points below:
- Give headlines and brief descriptions to maximise the time available.
- Ensure your presentation is clear and well-structured.
- One-minute time limit - Your presentation must last for no more than one minute, and you will be stopped at this point.
- No aids/resources allowed – you are not allowed to use any visual representations, such as PowerPoint, when giving your presentation and you must not share your screen. You are welcome to use notes, but these should be for your own use only.
Not an actual question, you will be assessed and scored specifically on the communication skills you demonstrate throughout the station.
This will be both an assessment of how you would communicate with patients, colleagues, etc. in the scenario, as well as of how well you communicate with interviewers throughout all questions.
This question will focus on your suitability for and commitment to training in the specialty and give you an opportunity to expand on the information provided in your application form.
This question will last approximately 10 minutes.
For this question, you will need to give a presentation on the following topic, for no more than five minutes:
'An interesting recent development / research finding, relevant to clinical pharmacology & therapeutics'
When preparing your presentation, please bear in mind the points below:
- Clarity & relevance most important - The major purpose of this question is to assess your understanding of the specialty and your communication skills. Thus you should select a topic that is relevant to CPT, and which you can present with clarity. This is more important than trying to impress by choosing a subject that is esoteric or complex. The topic should be relevant to your application where possible.
- Five minute time limit - Your presentation must last for no more than five minutes. Please note that you will be stopped after five minutes so as to allow further discussion to take place, so try and get your main points across before then. At the same time, bear in mind that interviewers will be assessing the level, depth and content of your presentation, as well as expecting some structure.
-
No aids/resources allowed – you are not allowed to use any visual representations, such as PowerPoint, when giving your presentation and you must not share your screen. You are welcome to use prompts on small cards, but these should be for your own use only.
Interview nerves will be taken into consideration.
Post-presentation discussion
Once your presentation is finished (interviewers will stop you at the five minute-mark), interviewers will discuss it with you and ask further questions relating to the items you raise and any further points.
Research & academic medicine discussion
Once your presentation and the subsequent discussion is finished, you will then move onto a general discussion on the subject of research and academic medicine.
No specific preparation will be required of you here, and you will not receive data in advance as you did with the clinical scenario.
However, we would advise undertaking some general preparation. For example, familiarising yourself with the process by which medical research takes place and progresses, from initial setup to report; as well as any areas of research that interest you, and the challenges, benefits, costs, etc. of research more broadly.
Areas for assessment
You will be scored on a combination of your presentation and its accompanying discussion; and your knowledge, awareness and understanding of medical research.
As noted, the presentation should last for no more than five minutes. The remaining five minutes will be split between the presentation discussion and the research/academic medicine discussion as is required.
Not an actual question, you will be assessed and scored specifically on the communication skills you demonstrate throughout the station.
Scoring framework
The score of 1-5 an interviewer will award you for each assessment area is judged in relation to how well you perform against an expected level. Below is the framework used to award scores at interview, as well as interpretation of what these scores represent:
|
Mark
|
Rating
|
Assessment
|
|
1 |
poor |
not considered appointable |
|
2 |
area for concern |
performed below the level expected from a core level trainee applying to the specialty; |
|
3 |
satisfactory |
performed at the level expected of a core level trainee applying to the specialty; |
|
4 |
good |
above average ability; |
|
5 |
excellent |
highly performing trainee; |
As shown in the table, for each of the question areas at interview, 3/5 is considered a satisfactory score; and reflects the level of performance that would be expected of a trainee ready to progress to a specialty training programme.
Should your performance go above and beyond this expected level, interviewers can award marks of 4/5 or 5/5 as appropriate.
Conversely, should your interview performance not reach the expected level, then interviewers can award marks of 1/5 or 2/5, as reflects their level of concern over your performance.
Appointability
Raw interview score (RIS)
The RIS is the sum of all twelve scores awarded to you during your interview, but before any weighting is applied.
As each individual score will be between 1 and 5, your RIS will be between 12 and 60.
Appointability requirements
To be classed as 'appointable', you must meet all three criteria below:
- none of your twelve interview scores can be 1/5
- no more than two of your twelve interview scores can be 2/5
- your RIS must be 36 or above.
If you meet all three requirements, your application will be assessed as appointable, and can progress to be considered for post offers.
However, if you fail to meet any of these requirements, your application must then be assessed as not appointable, and it will progress no further in that round.
Total score
After interview, a weighting is applied to the scores in each area, as well as your application score.
These scores are then combined to give your total score which determines your ranking, which will in turn be used to inform how offers are made. The weighting of different sections, as well as the method by which your total score is established, is detailed in the table accessible through the link below:
|
|
Interviewer 1
|
Interviewer 2
|
Weighting
|
Max score
|
|
Question 1 |
||||
|
Clinical scenario |
/ 5 |
/ 5 |
1.6 |
16 |
|
Question 2 |
||||
|
Medical registrar suitability |
/ 5 | /5 | 1.2 | 12 |
|
Question 3 |
||||
|
Communication mark |
/ 5 |
/ 5 |
1.2 |
12 |
|
Question 4 |
||||
|
Suitability and commitment |
/ 5 |
/ 5 |
1.6 |
16 |
|
Question 5 |
||||
|
Presentation/Research/Academic |
/ 5 | / 5 | 1.6 | 16 |
|
Question 6 |
||||
|
Communication mark |
/ 5 | / 5 | 0.8 | 8 |
|
Raw interview score |
/ 50 |
|||
|
Interview score (w weighting) |
/ 80 |
|||
|
Application score |
/ 40 |
0.5 |
/ 20 |
|
|
Total score |
/ 100 |
|||