Medical oncology is a dynamic and rapidly evolving speciality which involves both cutting edge research and a commitment to the care of a varied and often complex patient group.It is an exciting specialty, centred around patient care and the delivery of systemic anti-cancer therapy (SACT). There is also significant potential for furthering other aspects of your career, including research, leadership and management, training and education, and quality improvement.
Medical oncology trainee characteristics
Medical oncology will particularly suit trainees who:
- have good communication skills
- enjoy practising evidence-based medicine; by analysing and adapting the results of recent research in order to optimise patient outcomes
- are interested in a broad spectrum of academic research, including basic and translational science and clinical trials
- can work as part of a multidisciplinary team, including surgical oncologists, clinical oncologists, palliative care physicians, radiologists, pathologists, and clinical nurse specialists, as well as other medical specialties who support the management of toxicity from SACT.
Working in medical oncology
Half of the UK population will develop cancer during their lifetime, and this is predicted to increase as the population ages. Cancer treatment has advanced significantly during the 21st century, with the ability to give increasingly personalised targeted therapies, treatments such as immunotherapy, alongside the backbone of chemotherapy. As a result, patients are now living longer with cancer. Nevertheless, there is still a pressing need for improvement in cancer care, and medical oncologists are at the forefront of these improvements.
Medical Oncology trainees will develop the skills to be able to deliver systemic anti-cancer therapy (SACT) to patients with a wide variety of cancer types, and at various stages in their cancer journey. The delivery of SACT requires trainees learn how to integrate cancer-specific and patient-specific information, based on the latest research, to deliver individualised treatment, aiming to improve quality of life and cancer outcomes whilst trying to minimise (and effectively manage) any complications from the treatment or the underlying cancer.
Medical oncologists are an essential part of cancer multi-disciplinary teams, working closely with surgeons, clinical oncologists, radiologists, palliative care physicians and clinical nurse specialists. Newer therapies have also led to multiple different organ complications, requiring close input with many other specialties to effectively manage these toxicities.
Recognising the increasing impact of cancer on all aspects of the healthcare system, oncologists are playing a key role by leading Acute Oncology services. These services support general medical services by providing expert input for unplanned admissions with complications of cancer or cancer therapy. This is an expanding aspect of Medical Oncology for those trainees interested in maintaining a close link with general medical services.
As one the 2 main specialties providing non-surgical oncology care, Medical Oncologists work together with Clinical Oncology (which specialises in the delivery of radiotherapy) to provide all aspects of cancer therapy. Recognising the similarities in practice, the 2 specialties now have a Combined Oncology Stem during ST3, which gives Medical Oncology trainees greater experience in the delivery of radiotherapy in cancer treatment.
Underlying cancer care is the role of research in improving outcomes. The UK has always been at the forefront of cancer research, from the very basics of understanding how cancer develops and progresses, to large-scale clinical trials of new drugs to improve patient outcomes. To this end, many medical oncology trainees will take time out during their training to pursue a higher degree (MD or PhD), although this is not an essential part of being a successful medical oncologist. Apart from research, there is also tremendous scope for development in leadership and management, training, education, and quality improvement.
Medical Oncology provides an exciting career where no two days are the same. It is an expanding specialty, which will allow for greater collaboration across the country and allow the specialty to help direct the future of cancer care. If you would like to hear from current StR and Consultants on what a career in Medical Oncology entails, please view the recently recorded webinars on the Association of Cancer Physicians website (link below). Overall, this is a great time to consider medical oncology as a career.
Further information
- NHS health careers - medical oncology
- JRCPTB specialty page and curriculum
- ST3 medical oncology person specification
- Association of Cancer Physicians Careers Advice
General / application queries
For general queries relating to areas such as eligibility criteria, making an application or the Oriel system, please contact the Physician Specialty Recruitment Office.
Queries regarding the progress of a submitted application should be directed to the lead recruiter for this specialty. The lead recruiter for medical oncology is the London Recruitment Office:
| London Recruitment Office | ||||||
|---|---|---|---|---|---|---|
| HST/general queries | General enquiries - Enquiry Form | |||||
| Fitness to practise - confidential | Fitness to practise | |||||
Sometimes participates in round 2
This specialty’s participation in the second round is uncertain until after the first round is completed. Participation in the second round is confirmed in June each year.
Group 2 specialty
This is a Group 2 specialty and requires completion of the first two years of the internal medicine training (IMT) stage 1 programme or equivalent. Please visit the am I eligible? section of this website for further information about the eligibility criteria for Group 2 specialties.
Commitment to specialty
The specialty will be assessing your commitment to specialty as part of the shortlisting process. Please visit the application scoring page for more information about how this is assessed and scored.
Indicative post numbers
Indicative vacancy numbers are available in the table below, broken down by region and divided between substantive national training number (NTN) and locum appointment for training (LAT) posts. In many cases these will be presented as a range (e.g. 1-4) as it is not always possible for regions to know at this stage how many vacancies there will be.
It is the intention that indicative post numbers for all regions will be published prior to the application opening date, although this cannot be guaranteed. Please note that this table is not likely to be updated subsequent to indicative numbers and actual numbers will be confirmed when programme preferences are opened later in the round.
Numbers subject to change
Please be aware that it is not uncommon for vacancy numbers to change as the round progresses.
More commonly, post vacancy numbers can increase as the round goes on (and confirmation of posts becomes available); but it is also possible that numbers can reduce as well. In the past, post numbers have risen an average of 20-40% from the start to the finish of the round but this can vary greatly for individual specialty/region combinations.
It is possible that regions which do not have a post at the start of the round may declare one after applications have closed. Whilst we try and minimise instances of this, it is not always possible to predict vacancies so even if there appears not to be a vacancy in your preferred specialty/region combination, you may wish to consider applying in case one becomes available during the round; you can check with the region concerned if you wish to check on the likelihood of a post arising.
Generally, once a region enter a post into a round they would always have at least one post available and would only withdraw it in exceptional circumstances.
Round 1 Interview dates & posts
| Region |
NTN posts
|
LAT posts*
|
Evidence upload date(s) | Interview date(s) |
|---|---|---|---|---|
| East Midlands | 1 - 4 | N/A |
15/12/25 - 12/01/26 |
19, 20 March 2026 |
| East of England | 0 - 2 | N/A | ||
|
London |
2 - 13 | N/A | ||
| Kent, Surrey and Sussex | 0 - 2 | N/A | ||
| North East | 0 - 2 | N/A | ||
| North West |
North West 0 - 1 Mersey 0 - 1 |
N/A | ||
|
South West |
Severn
2 - 5
|
N/A | ||
|
Peninsula
1 - 2
|
N/A | |||
| Thames Valley | 0 - 1 | N/A | ||
| Wessex | 1 - 3 | N/A | ||
| West Midlands | 3 - 5 | N/A | ||
| Yorkshire & Humber | 0 - 1 | N/A | ||
| Northern Ireland | 0 - 2 |
TBC
|
||
| Scotland** | 1 - 6 |
TBC
|
||
| Wales | 1 - 2 |
TBC
|
*English LATs
Please note, English regions do not recruit to LAT posts.
**Scotland post numbers
If you are interested in working in Scotland, a breakdown of post numbers by the four Scottish regions is available on the Scottish Medical Training website. This has details of all specialty training post numbers in Scotland, including specialties which are not part of the nationally-coordinated process.
The SMT website will always be the more accurate one where they differ.
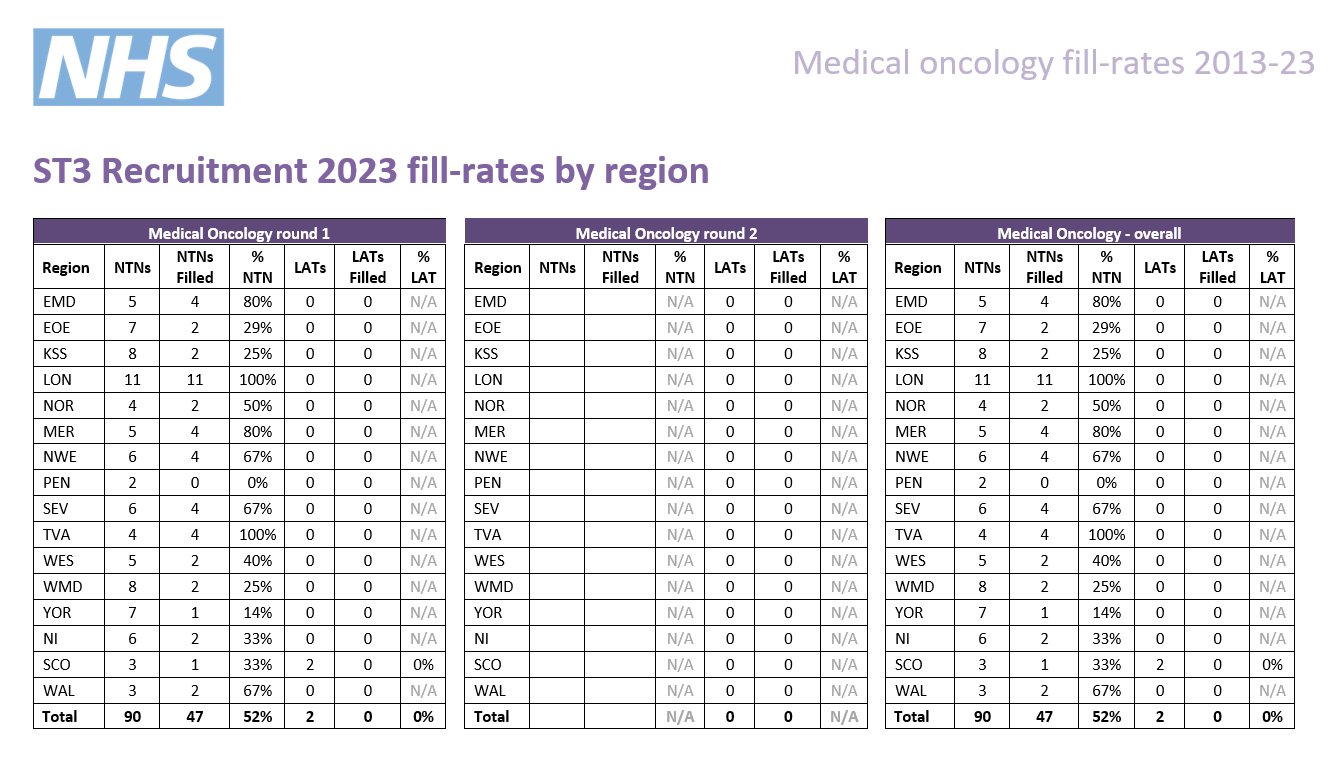
As part of the process of applying to HST, you may wish to gain an idea of how recruitment progressed in previous years for the various specialties participating in the nationally-coordinated recruitment.
To this end, we have published data dating back to 2013 (where this is available), based around four main areas:
-
Competition ratios - application numbers submitted to each specialty, along with the number of NTN and LAT posts available in each. It is worth noting that posts are subject to change throughout the round (increasing on average between 20-40%), and post numbers for this data are taken at the end of the round.
-
Shortlist scores - the scores awarded to all submitted applications, including average scores and distribution nationally.
-
Total scores - the total score awarded to all candidates who completed the full recruitment process for a specialty (application and interview), including some analysis of scores.
-
Post fill rates - the number of posts filled by region.
We have published information for all specialties participating in our process that year; consequently not all specialties will have data in all cases.
Round 1
| Year | Apps. | NTN posts | LAT posts | Total posts | Comp. | Unique* |
|---|---|---|---|---|---|---|
| 2025 | 319 | 91 | 0 | 91 | 3.5 | 55% |
| 2024 | 265 | 90 | 0 | 90 | 2.9 | 61% |
| 2023 | 187 | 90 | 2 | 92 | 2.1 | 55% |
| 2022 | 214 | 88 | 0 | 88 | 2.4 | 63% |
| 2021 | 212 | 79 | 1 | 80 | 2.6 | N/A*** |
| 2020 | 185 | 36 | 1 | 37 | 5 | 64%** |
| 2019 | 151 | 38 | 1 | 39 | 3.9 | 70%** |
| 2018 | 121 | 53 | 2 | 55 | 2.2 | 69%** |
| 2017 | 114 | 54 | 0 | 54 | 2.1 | 64%** |
| 2016 | 122 | 55 | 4 | 55 | 2.2 | 36% |
| 2015 | 110 | 35 | 13 | 48 | 2.3 | 25% |
*the percentage of unique candidates that only applied to this specialty (out of the PSRO-coordinated specialties).
**Since 2017 not included candidates that also applied to clinical oncology as the data was not available; it is likely that had this been available the percentage would have been similar to 2015/2016.
*** As many specialties did not participate in recruitment in 2021, the data is not comparable.
Round 2
| Year | Apps. | NTN posts | LAT posts | Total posts | Comp. |
|---|---|---|---|---|---|
| 2023 |
85 |
47 | 0 | 47 | 1.8 |
| 2022 |
54 |
22 | 1 | 23 | 2.3 |
| 2021 |
This specialty did not participate in round 2 between 2017 and 2021 |
||||
| 2020 | |||||
| 2019 | |||||
| 2018 | |||||
| 2017 | |||||
| 2016 | 17 | 17 | 1 | 18 | 0.9 |
Interview content
The interview will be split across two stations with a separate pair of interviewers scoring you on the areas in their station. There will be four questions which range between 5-6 minutes in length. You will be scored by two interviewers on each question.
Each station will last 11 minutes, so including the time between stations, the interview will be approximately 30 minutes.
Please note that this is subject to change and will be confirmed by the date of interview.
Immediately prior to the start of the interview, you will be given a clinical scenario to review; you will have a short while to review the scenario. You will then have approximately 6 minutes where the panel will ask you questions regarding the scenario.
The clinical scenario will be relatively brief (two/three sentences), so once you have seen this, the remainder of the preparation time will allow you to undertake some short mental preparation. Whilst it is permitted to make notes, these must be destroyed as soon as your interview is completed and not shared with anyone.
Scenario considerations
The scenario will describe a hypothetical clinical situation which has arisen in which you are, or have become, involved. Some points to consider when reviewing the scenario and preparing for discussion are:
- what steps you would take
- any potential treatments possible
- any further information you would gather
- how you would go about communicating with any people (eg patients, family members, colleagues) involved in the scenario.
You should take into account any other factors you deem appropriate, using your experience and professional judgement.
This question will explore ethical, professionalism and governance issues. It will start with a hypothetical situation which is not given to you before entering the station and will be given verbally by interviewers.
This is not a clinical question, but will deal with the moral, ethical, legal, etc. issues of a particular situation. Following the hypothetical situation, and where time allows, there will be one or more questions about GMC Good Medical Practice principles.
The assessment of this question is underpinned by the principles of GMC Good Medical Practice.
This question will last approximately 5 minutes.
This question will focus on your suitability for and commitment to ST3 training in the specialty and give you opportunity to expand on the information provided in your application form.
This question will last approximately 6 minutes.
This question is a general discussion on the subject of research and academic medicine. The question will last for approximately 5 minutes.
No specific preparation will be required of you here, and you will not receive information in advance as you did with the clinical scenario.
However, we would advise undertaking some general preparation. For example, familiarising yourself with the process by which medical research takes place and progresses, from initial setup to report; as well as any areas of research that interest you, and the challenges, benefits, costs, etc. of research more broadly.
Scoring framework
The score of 1-5 an interviewer will award you for each assessment area is judged in relation to how well you perform against an expected level. Below is the framework used to award scores at interview, as well as interpretation of what these scores represent:
|
Mark
|
Rating
|
Assessment
|
|
1 |
poor |
not considered appointable |
|
2 |
area for concern |
performed below the level expected from a core level trainee applying to the specialty; |
|
3 |
satisfactory |
performed at the level expected of a core level trainee applying to the specialty; |
|
4 |
good |
above average ability; |
|
5 |
excellent |
highly performing trainee; |
As shown in the table, for each of the question areas at interview, 3/5 is considered a satisfactory score; and reflects the level of performance that would be expected of a trainee ready to progress to a specialty training programme.
Should your performance go above and beyond this expected level, interviewers can award marks of 4/5 or 5/5 as appropriate.
Conversely, should your interview performance not reach the expected level, then interviewers can award marks of 1/5 or 2/5, as reflects their level of concern over your performance.
Appointability
Raw interview score (RIS)
The RIS is the sum of all eight scores awarded to you during your interview, but before any weighting is applied.
As each individual score will be between 1 and 5, your RIS will be between 8 and 40.
Appointability requirements
To be classed as 'appointable', you must meet all three criteria below:
- none of your eight interview scores can be 1/5
- no more than two of your eight interview scores can be 2/5
- your RIS must be 24 or above.
If you meet all three requirements, your application will be assessed as appointable, and can progress to be considered for post offers.
However, if you fail to meet any of these requirements, your application must then be assessed as not appointable, and it will progress no further in that round.
Total Score
|
|
Interviewer 1
|
Interviewer 2
|
Weighting
|
Max score
|
|
Question 1 |
||||
|
Clinical scenario |
/ 5 |
/ 5 |
2.5 |
25 |
|
Question 2 |
||||
|
Professionalism & governance |
/ 5 |
/ 5 |
1.8 |
18 |
|
Question 3 |
||||
|
Suitability & commitment |
/ 5 |
/ 5 |
1.2 |
12 |
|
Question 4 |
|
|||
|
Academic/research |
/ 5 |
/ 5 |
2.5 |
25 |
|
Raw interview score |
/ 40 |
|||
|
Interview score (w weighting) |
/ 80 |
|||
|
Application score |
/ 40 |
0.5 |
/ 20 |
|
|
Total score |
/ 100 |
|||